Reinventing 3D printed tourniquets for Ukraine is a mistake
Makers and volunteers must stop producing 3D-printed tourniquets with known design and production flaws and use field-tested designs and procedures. One such field-tested open source design is Glia’s Gaza Tourniquet, and there are several widely-used closed-source designs such as the Combat Application Tourniquet (CAT) and SOF-T tourniquet. Quality assurance procedures specific to medical devices such as those by Health Canada (see below), FDA, CE or ISO must also be adhered to.
Makers and volunteers have taken up calls by Ukrainian health care workers to provide medical support, supplies and aid. It is heartwarming to see people across the world ensuring everybody in Ukraine can receive excellent medical care.
There are ongoing efforts to create and distribute tourniquets in response to these calls. Several groups are making easily-identified and easily-correctable mistakes that may unnecessarily endanger patient safety, resulting in potential injury or death. After careful consideration, and seeing as working open source alternatives currently exist, we call on all groups:
- To cease production and distribution of tourniquet designs with known design and production mistakes like those below immediately until these errors are corrected.
- To cease production and distribution of novel tourniquet designs in Ukraine until they are carefully tested in non-battlefield conditions.
Below, I discuss some design considerations that must be taken into account when making a tourniquet. I will try to make this article exhaustive, and will add other parts later if necessary, so don’t hesitate to send feedback. In it, I catalogue Glia’s journey and the many mistakes we made along the way with the hopes that they are never made again.
Why Gazans are experts at 3D printed tourniquets
Glia was founded in 2013 as a result of the 2012 war on Gaza, and we have been systematically addressing problems in high quality local manufacture of medical devices since then. Glia’s first 3D-printed tourniquet was released to the world on February 27, 2017. We deployed it to the field as an emergency use device just over a year later and reported on our progress and findings here and here.
We invested countless hours along with Gaza’s four paramedic services, hospitals and ministries to refine the design. Glia’s Gaza Tourniquet has been used on hundreds of gunshot, explosives and trauma victims with no recorded technical failures in 46 months. This includes usage during the 2018–2020 Great March of Return in which 5,969 people shot (86.9% in the arms or legs). Despite this, only 2 died of their injuries, a remarkably low 0.03% fatality rate. The tourniquets were also used during the 2021 war on Gaza. The tourniquets’ performance has been monitored as carefully as is possible during war. Gaza is a caustic austere health care environment that serves as an acid test for any project.
Glia is also based in Canada and holds a Health Canada Medical Device Establishment License (License #6823) to produce Class 1 devices such as the tourniquet. We are also actively developing several Class 2 devices. Want to get your own MDEL? We open sourced all of our regulatory documents. Our work is published in a peer-reviewed publication on a 3D printed stethoscope (2018), and we have given numerous presentations at academic and non-academic conferences.
As for me personally, I am an emergency medicine consultant physician based in Canada. I hold an associate professorship at the University of Western Ontario and am an associate Scientist at Lawson Health Research Institute. I work in Gaza’s Dar al-Shifa Hospital, and was there during the 2012 war and part of the 2014 war. I actively developed the tourniquet during the 2018–2020 Great March of Return, where I was shot through both legs while providing care to other victims.
A lack of deep contextual knowledge
We made every mistake I’m seeing in de novo tourniquet designs currently being proposed. I see us all as being friends on the same team: we see the same problem and want to help. Despite the best intentions, some makers are making easily identified, easily corrected mistakes.
As Alix Dunn articulated beautifully in a thread published at the beginning of the war on Ukraine, “‘Cool ideas’ coming from a place of limited contextual knowledge can be dangerous. Spinning up tech that is unmoored from institutions and infrastructure is superficial and unsustainable.” She continued with an observation we see in every crisis: “In hard times, technology is intoxicating. It can feel like a shortcut to impact in a moment of impossible hardship.” She concludes that thought by reminding us: “It’s not.”
The Glia team had conversations with at many designers and reviewed at least 10 de novo designs and numerous suggested modifications to Glia’s current design. Almost all of the de novo designs make them, and we did too. Some makers have been open to making modifications based on Gaza’s experience and knowledge; others are rushing to deploy into the field despite easily-addressed safety concerns.
Making the same mistakes
Most of the new designs we’ve reviewed make the same mistakes. I’ve addressed those that are easily addressed to highlight the mistakes Glia made that are being repeated. My perspective is informed by conversations with makers, all of whom share significant commonalities.
Engineering and printing decisions do not trump safety and usage considerations: Cylindrical windlasses
Take a look at every windlass (the rod you twist in a tourniquet) on the market. Notice something? They’re all cylindrical.

Designers know cylinders are hard to print on 3D printers, so their first instinct is to facet the design to create a surface to print on. Every de novo design does this. And yes, that included Glia. Take a look at our first design, which we started testing more than 5 years ago in February, 2017 as compared to many of the de novo design windlasses.
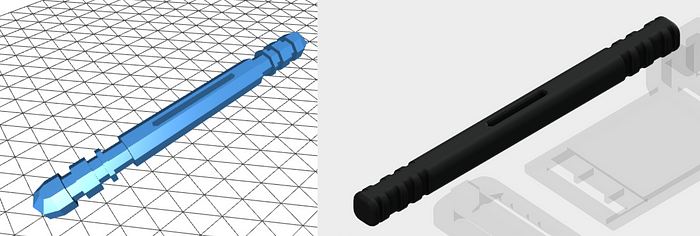
When we tested faceted designs, we found a few problems:
- The diameter of the windlass is not constant depending on rotation, meaning that the design has to either accommodate the biggest diameter or the smallest diameter. The more facets, the closer those numbers are. With equilaterals, this difference is most dramatic in a triangle (Δr = a√3/2 – a), and least dramatic in a cylinder (Δr = 0). A square shape like above is the second-largest difference (Δr = √(2a²) – a). Clinically, we found that the subtle problems caused by these design choices mean that time for application and securing of tourniquet is increased by several seconds (target application time = 20 seconds).
- The lack of grooves at all parts of the windlass makes it less likely to stay in place during operation. Some designs have no grooves at all. During some small field tests, this resulted in clipping failures, and was largely remedied by ensuring grooves at all contact points.
Printing a non-cylindrical windlass is not recommended, even for emergency use. Experiments on more printable versions have started, but require significant work before they are ready for patients.
Duplicating the CAT duplicates its shortcomings

Makers are — somewhat sensibly — looking at existing tourniquet designs for inspiration, just as the Glia team did when we started by duplicating CAT’s backing system in 2017. In the above case, copying the CAT v7 design violates one of North American Rescue’s key claims in US Patent #7892253B2 (Item 1.e) and US Patent#7842067 (item 8). There are exceptions to patent protection, and makers might argue that the crisis in Ukraine justifies violating NAR’s patent.
This design choice resulted in a bigger issue: it increased clinical failures in patients with smaller limbs, which disproportionately affects women and children. Since ~45% of Gaza’s population is under the age of 14, and slightly over half of adults are women, this was a serious concern. We found that by making two small changes, we increased the effectiveness of Glia’s Gaza tourniquet on those with smaller limbs: separating the clip and backing support; and thinning the backing support to make it more pliable.
PLA is the wrong material; PETG is probably OK; ABS should be used
PLA is a nice plastic that’s fun to play with and use. It’s easy and most of its properties are suitable for makers. That’s why Glia started with PLA in 2017. We discovered what everybody who’s walked our path already knows: PLA is not suitable for outdoor use, nor for situations where storage conditions cannot be controlled. We switched to using ABS, which remains the right material for Gaza.
When the Ukraine crisis began, makers questioned whether PETG could be used to print tourniquets. Glia has been testing PETG for the past 4–5 months. UPDATE: As of March 25, 2022. Glia has approved PETG for use in tourniquets. More details to come soon.
Where ABS is not possible to use, PETG may be used so long as it is stored away from humidity and UV after production, such as in sealed plastic. As most of these are expected to be in individual first aid kits (IFAKs) and generally be away from the sun, we expect they should perform well after storage.
That brings us to the perplexing re-emergence of PLA for printing tourniquets today. I have discussed this question with our engineers and we see no evidence that the fundamentals of PLA have changed. Glia’s advice remains to never use PLA for production tourniquets.
Most makers do not have experience with how tourniquets works
Most makers don’t have experience with how tourniquets work, and that’s OK so long as they’re open to feedback. When they are not, this lack of deep contextual knowledge means making wrong assumptions and mistakes.
Here’s an example: Glia received the following video without commentary from one maker. This looks like a critique of how pliable the backing plate is. I wasn’t able to get clarification on what the video was trying to show, but the implication is clear: Because Glia’s Gaza Tourniquet backing plate is pliable, it is bad.

This critique is concerning, since it implies the makers behind it don’t understand that the part should be pliable. If the resulting design is stiffer, it may result in unnecessary harms due to uneven distribution of pressure and dead spots in the tourniquet’s pressure distribution.
Most of the changes we’ve proposed over the past few weeks stemmed from designers and makers not having a clear understanding of how tourniquets should work. That’s totally OK —Glia learned lots about tourniquets over the past 6 years with many revisions and field trials. While the lack of deep contextual information isn’t itself a problem, unfounded confidence in bad design choices is.
Safety first; Speed second
We’re all worked up and passionately committed to helping those who are suffering around us — I haven’t run into many bad intentions in the maker community. That motivation mixed with the collective traumas we continue to face can sometimes lead us to think two dangerous thoughts: “right now” and “something is better than nothing”.
When it came to face shields, PPE and prosthetics, mistakes did not have the potential to be so instantly catastrophic. In early 2018, I had one of Glia’s tourniquets fail in my hand in the field when treating a gunshot victim. The panic of thinking that my failed device might be partly responsible for a patient’s bad outcome is something I don’t wish upon anybody. The potential ethical and moral injury to makers is a real concern.
When Glia started, there was no depth of open source knowledge and no expertise for us to find in the open or scientific community about producing tourniquets. Now there is. Let’s all use it and avoid making the same mistakes again.
How you can help
If you have any questions, don’t hesitate to contact us at info@glia.org or through Glia’s Web, Twitter or Facebook pages. If you have deep expertise in tourniquet construction or design and are willing to share, please be in touch and we’ll post your information here.
If you wish to contribute financially, the International Committee of the Red Cross (ICRC) is accepting donations, and of course you can contribute to Glia’s ongoing campaign to produce tourniquets in Ukraine and import them to Ukraine from Gaza, Canada and elsewhere.
If you are a maker, we have found several networks that we feel are navigating the balance of speed and quality carefully, including Open Source Medical Supplies and a few other networks. Reach out to one of these networks to if you have expertise in 3D printing, sewing, logistics, or health care.
If you are a designer, we are happy to give feedback on your design.
Acknowledgements: Dr. Mohammed Al-Attar, who has been the on-the-ground lead and asked Glia to develop the tourniquet in 2016. Alix Dunn, who gave language to our observations and concerns in an excellent thread. Musa Abuhassanin, who lost his life while courageously caring for gunshot victims and using Gaza tourniquets. The numerous medics, engineers and physicians in Gaza who contributed feedback, advice and refinements. The victims of war and oppression everywhere.
